What Is The Criteria To Have Your Bladder Repair
Pelvic Prolapse Repair
For many women, prolapse tin can include descent of the uterus, vagina, bladder and/or rectum resulting in a "bulging" sensation within the vagina. In some cases, frank protrusion of these organs can occur. Pelvic organ prolapse tin can result in symptoms including urinary leakage, constipation, and difficulty with intercourse.
Laparoscopic colposuspension is a minimally invasive surgical technique that provides a safe and durable method for reconstruction of the pelvic flooring and its contents without the need for a large abdominal incision.
The Surgery
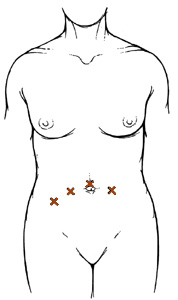
Laparoscopic colposuspension is performed using fine laparoscopic instrumentation inserted through iv keyhole incisions beyond the mid belly (Figure one).
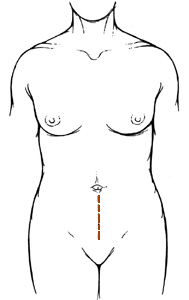
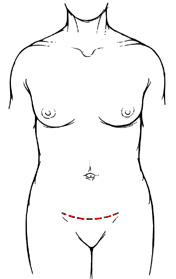
This is in contrast to the conventional open intestinal colposuspension where a lower midline (Effigy 2a) or Pfannenstiel (Figure 2b) abdominal incision is required.
In cases of pelvic organ prolapse, at that place is laxity of vaginal support resulting in protrusion of the pelvic organs. The goal of laparoscopic colposuspension is to resuspend the vagina and associated pelvic organs through the cardinal-pigsty incisions. In certain circumstances, a simultaneous hysterectomy, float suspension, or rectocele repair may exist required, all of which can be accomplished through a vaginal approach.
Laparoscopic colposuspension is a well established procedure at Johns Hopkins Bayview Medical Heart and is performed with the aid of an experienced and defended laparoscopic surgical team including nurses, anesthesiologists, operating room technicians, many of whom you will meet the mean solar day of surgery.
Laparoscopic colposuspension is performed through 4 small keyhole (0.v-1 cm) incisions across the mid abdomen (Effigy 1). Through these small incisions, fine laparoscopic instruments are inserted to dissect and suture. Excellent visualization of the pelvic organs is achieved with the apply of a high-powered telescopic lens attached to a camera device, which is inserted into one of the keyhole incisions.
The vagina and pelvic organs are then resuspended internally with a combination of sutures and a supportive mesh or fascial graft (Figure iii). If needed, a bladder suspension, vaginal hysterectomy, and rectocele repair can exist accomplished at the same time via a vaginal incision. A Foley catheter (i.due east. bladder catheter) is placed to drain the float. A gauze vaginal packing is also placed at the end of the procedure.
The length of operative time for laparoscopic colposuspension can vary greatly (three-5 hours) from patient to patient depending on the internal anatomy, shape of the pelvis, weight of the patient, and presence of scarring or inflammation in the pelvis due to infection or prior intestinal/pelvic surgery.
Blood loss during laparoscopic colposuspension is routinely less than 200 cc and transfusions are rarely required.
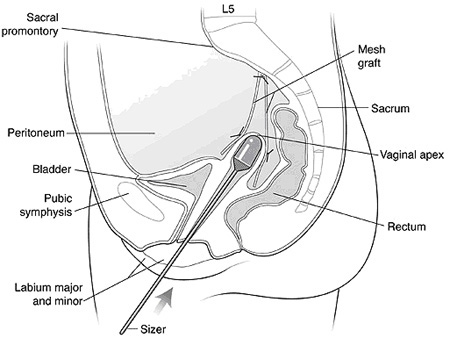
Figure 3. Schematic sagittal view of laparoscopic colposuspension with mesh graft.
Potential Risks and Complications
Although laparoscopic colposuspension has proven to be very safe, as in any surgical procedure there are risks and potential complications. Potential risks include:
-
Haemorrhage: Although claret loss during this process is relatively low compared to open surgery, a transfusion may still exist required if deemed necessary either during the operation or afterwards during the postoperative period.
-
Infection: All patients are treated with intravenous antibiotics, prior to the commencement of surgery to decrease the chance of infection from occurring inside the urinary tract or at the incision sites.
-
Adjacent Tissue / Organ Injury: Although uncommon, possible injury to surrounding tissue and organs including bowel, vascular structures, pelvic musculature, and nerves could require farther procedures. Transient injury to nerves or muscles tin can as well occur related to patient positioning during the functioning.
-
Hernia: Hernias at the incision sites rarely occur since all keyhole incisions are closed under directly laparoscopic view.
-
Conversion to Open Surgery: The surgical procedure may require conversion to the standard open operation if extreme difficulty is encountered during the laparoscopic process (e.g. excess scarring or bleeding). This could result in a standard open incision and perhaps a longer recuperation period.
-
Urinary Incontinence: Pre-existing urinary incontinence volition typically be addressed at the time of surgery with a bladder sling suspension, however, small incontinence may nevertheless be, which typically resolves with time. On occasion, medication may be required.
-
Urinary Retention: As with urinary incontinence, postoperative urinary retention is uncommon and unremarkably is present in patients who undergo concurrent float sling intermission. Temporary intermittent self-catheterization may be required postoperatively.
-
Vesicovaginal fistula: A fistula (abnormal connection) betwixt the bladder and vagina is a rare complication of any pelvic surgery involving the vagina, uterus, and float. A vesicovaginal fistula typically manifests with symptoms of continuous urinary leakage from the vagina. Although rare, these fistulas can be managed conservatively or by surgical repair through an vaginal incision.
Source: https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/pelvic-floor-repair
Posted by: kennywity1942.blogspot.com


0 Response to "What Is The Criteria To Have Your Bladder Repair"
Post a Comment